

NHS England has authorised a £120 million elective acceleration programme in what amounts to a final-quarter push to shift national waiting list performance before the March deadline. The funding, deployed as a concentrated sprint within existing allocations, is designed to drive rapid increases in outpatient appointments and procedures that generate measurable referral-to-treatment clock stops. With waiting list reduction at the centre of the government’s commitments, the operational stakes are unmistakable.
National RTT performance remains below the 65 per cent ambition set for March, sitting just above 61 per cent in the most recent publicly released NHS performance statistics. Closing that gap in weeks rather than months represents hundreds of thousands of pathways requiring resolution. The sprint funding is structured to reward activity delivered above planned levels in quarter four, meaning trusts will be supported for incremental elective output where baseline delivery has been achieved. In effect, NHS leadership is attempting to convert marginal capacity into visible performance movement at speed.
The strategic emphasis is deliberate. Between 70 and 80 per cent of elective patients conclude their care journey at first outpatient attendance or following a diagnostic-led procedure, according to NHS pathway data. By targeting that stage of the pathway, NHS England can maximise throughput and measurable RTT gains within a compressed timeframe. A portion of the funding will also be directed at patients waiting longer than 52 weeks, where over 140,000 cases remain within a national waiting list exceeding 7 million incomplete pathways, based on publicly available NHS England statistics.
The political context is explicit. Reducing waiting times was framed as a defining health priority at the last general election. Ministers have repeatedly stated that visible progress on elective recovery is essential. The sprint is therefore as much about confidence in delivery as it is about quarterly metrics.
Dr Penny Dash, chair of NHS England, has previously emphasised that elective recovery requires disciplined operational focus and clear accountability. In public remarks on system reform, she has underscored that improvement depends on sustained execution and transparency across providers. The current sprint is a direct expression of that philosophy: concentrated resource aligned to measurable outcomes.
The chart accompanying this article illustrates the concentration of incomplete pathways among the largest acute providers, using figures drawn from NHS England’s published RTT datasets. The scale is striking. Mid and South Essex and Manchester University Hospitals each carry backlogs approaching 180,000 pathways. Royal Free London, Northern Care Alliance and Barts Health each exceed 130,000. Even organisations performing comparatively well against the 18-week standard are managing incomplete pathways in excess of 80,000.
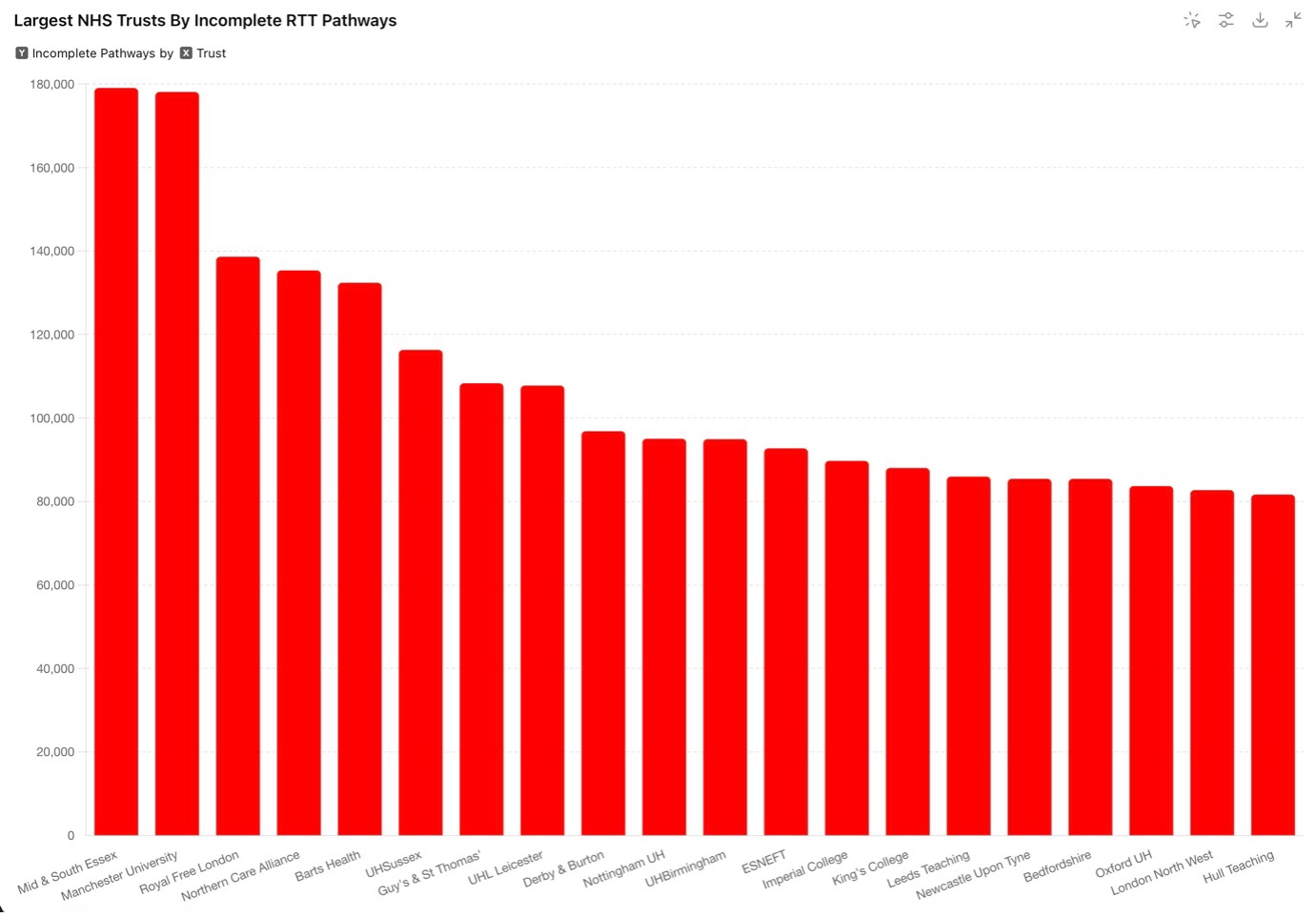
Performance variation is equally material. Some of the largest providers remain below 55 per cent of patients treated within 18 weeks, while others exceed 65 per cent and, in a few cases, approach or surpass 70 per cent. The disparity underscores that backlog size alone does not determine recovery trajectory. Operational configuration, clinical prioritisation, and pathway control matter.
For chief executives and chief operating officers, the sprint demands immediate tactical clarity. Where is outpatient elasticity still available. Which diagnostic bottlenecks can be cleared rapidly. How can theatre utilisation be optimised without undermining workforce resilience. The funding model presumes that performance headroom remains in the system. Whether that headroom can be unlocked at scale in the remaining weeks is the central operational question.
Complicating the equation are emerging supply pressures within trauma and orthopaedics, the largest specialty cohort on the elective waiting list. Publicly reported supply chain constraints affecting key surgical materials risk delaying a proportion of joint procedures. In isolation, these disruptions may appear modest relative to overall volumes. Within a compressed sprint environment, however, even marginal losses in high-volume specialties can blunt national trajectory.
The sprint is also running alongside ongoing validation efforts aimed at ensuring the waiting list accurately reflects active demand. Together, activity expansion and data validation are intended to sharpen both delivery and reporting integrity.
Ultimately, the £120 million acceleration is less about a single month’s statistics and more about institutional credibility. If the NHS can translate targeted funding into measurable RTT improvement within weeks, it reinforces the argument that disciplined operational execution remains the decisive lever of recovery. If it cannot, attention will shift from ambition to architecture.
For executive leaders, the message is clear. The backlog is concentrated. The metric is public. The timeframe is fixed. In the closing stretch of the financial year, performance will be judged not on narrative but on numbers.