

In 1863, the London Underground was formed to address a problem of scale. The city was growing faster than its streets could cope, and movement had become unpredictable. The answer was not more roads, but a system that could see, anticipate, and manage flow. Over time, that system evolved into more than 270 stations across 11 lines, carrying around five million passenger journeys a day through the capital with remarkable reliability.
Hospitals are now facing an equivalent moment.
At St George’s Hospital, around 150,000 patients pass through the emergency department each year, with tens of thousands more moving through inpatient beds. Serving a population of approximately 1.3 million people across south west London and beyond, St George’s is one of the busiest hospitals in the capital. The challenge it faces is not volume alone, but variability. Demand fluctuates. Length of stay shifts. Bottlenecks appear without warning.
For decades, hospitals have responded to this with reporting rather than prediction.
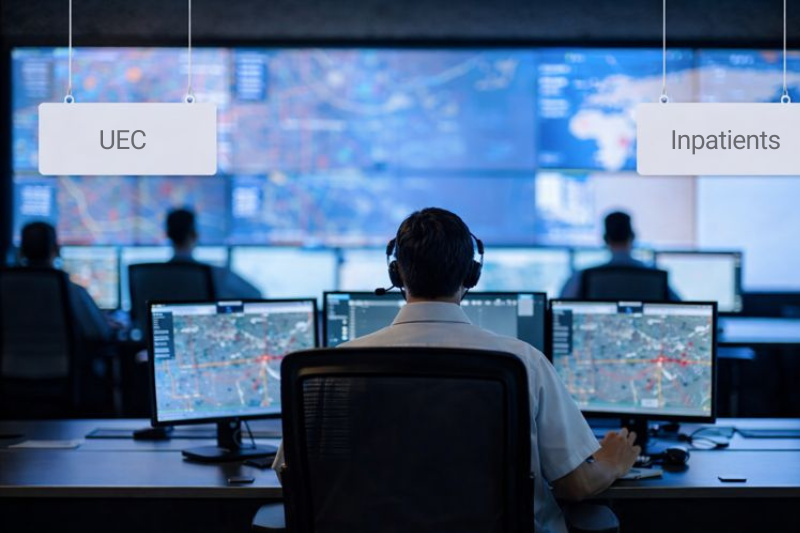
The brainchild of one of the most seasoned chief operating officers in the country, Tara Argent, the Georges Line represents a deliberate break from that past. It is not a dashboard in the conventional sense, but a real-time operational layer that treats the hospital as a data-driven system. It connects arrival, diagnostics, beds, discharge, and escalation into a single digital view of flow, refreshed continuously and visible to those who can act. It is a seamless blend of digital capability, data, early-stage AI, and physical operational infrastructure.

With prolonged industrial action over the past two years, demand and capacity have become defining challenges for the NHS and its leaders. Capacity constrained by tighter finances and rising demand is a difficult combination, creating sustained pressure and a clear need for new ways of thinking, working, and delivering. Recent ambulance delays have only compounded the problem, leaving many organisations struggling to regain control.
The Georges Line focuses on the urgent care pathway, where unpredictability is most acute and where every acute provider faces the same questions each day. How many patients are we expecting in A&E by 10am? How complex will demand be this week? What seasonal factors are driving it? How many patients can we discharge, and how many need to be safely sent home, and by when? Do we have the capacity and staff in place? Is cleaning ready? Are discharge summaries complete? What does patient experience look like today, and what are the infection control risks? These are the questions leadership teams across the country must answer daily to keep hospitals functioning.
What the Line provides is predictability. By aggregating live data streams and presenting them as a single operational truth, supported by early-stage AI, the Georges Line allows teams to see where pressure is forming before it becomes failure. Delays are no longer discovered retrospectively through reports. They appear as signals in the moment, allowing intervention while options still exist. You genuinely have to see it to believe it.
This shift mirrors what has happened in transport, energy, and finance. Systems once managed by experience and intuition are now governed by data, pattern recognition, and early warning. Healthcare has lagged behind, largely because its data has remained fragmented.
What ultimately sets the Georges Line apart is the person behind it. Tara Argent is the kind of operator you bring in when a hospital needs control, not commentary. She began her career at Eurotunnel, where safety, flow, and failure are brutally binary, then carried that discipline into senior NHS leadership roles at East Sussex Healthcare NHS Trust, Chelsea and Westminster NHS Foundation Trust, and Auckland District Health Board in New Zealand. As Chief Operating Officer at St George’s, she now sits over roughly 80 percent of hospital spend and almost all operational performance. Very few NHS leaders combine deep numerical command, systems engineering instinct, and frontline credibility. Fewer still can stabilise complex organisations under pressure. If a hospital needs saving, this is the calibre of leader you bring in to accelerate improvement in flow.
At St George’s, fragmentation has been deliberately removed. The impact is measurable. The trust has reduced length of stay, closed and kept closed 83 beds, and avoided routine escalation despite operating in one of the most pressured health economies in London. Using standard NHS assumptions, those closed beds are estimated to represent around 25,000 bed days removed from the system each year. On a conservative cost basis, this equates to an estimated £10–15 million of annualised value. From a leadership perspective, the value of the Line lies as much in confidence as in performance.
Tara Argent describes it as a shift away from managing by hindsight:
“Healthcare becomes hardest to manage when leaders are surprised by pressure. The Georges Line is about removing that surprise. It gives us real-time visibility across the whole organisation, turns delays into clear signals, and allows teams to act earlier, with confidence. That shift, from hindsight and firefighting to live control and accountability, is what changes outcomes.”
The Line has also changed how decisions are made. Nursing teams use it to identify and resolve delays themselves. Managers focus on interventions rather than explanations. Senior leaders use it as a live operational view rather than a retrospective account of yesterday’s problems.
What makes the Georges Line notable is that it does not rely on speculative AI claims. Instead, it creates the conditions in which predictive models can operate meaningfully. By standardising data and exposing flow clearly, it provides the foundation for more advanced analytics, forecasting, and automation. In that sense, the Georges Line is less a finished product than a new piece of infrastructure. Much like the early Underground, it establishes a framework on which future capability can be built.
As the NHS grapples with rising demand and constrained resources, the lesson from St George’s is not about technology alone. It is about designing healthcare systems that can see themselves clearly enough to predict, adapt, and move with confidence. The team is now working on a significant extension of this capability, with the potential to scale across the NHS. It is very much one to watch.