As the winter of 2025/26 grips the UK, the NHS is grappling with intense pressures in its emergency and acute care settings. This strain is most visibly and disturbingly manifested in the routine practice of care delivered in corridors, waiting rooms, and other non-clinical spaces. This widespread use of "escalation areas," once intended as temporary relief, has become endemic, sparking serious alarms over patient safety, dignity, and clinical standards. The scale of this problem is alarming: a major observational study in late 2025 showed that nearly one in five emergency department patients were receiving care in overflow spaces, a figure far exceeding national guidelines. Furthermore, a recent Royal College of Physicians snapshot survey found a staggering 78% of doctors reported providing care in unsafe or inappropriate spaces in the past month.
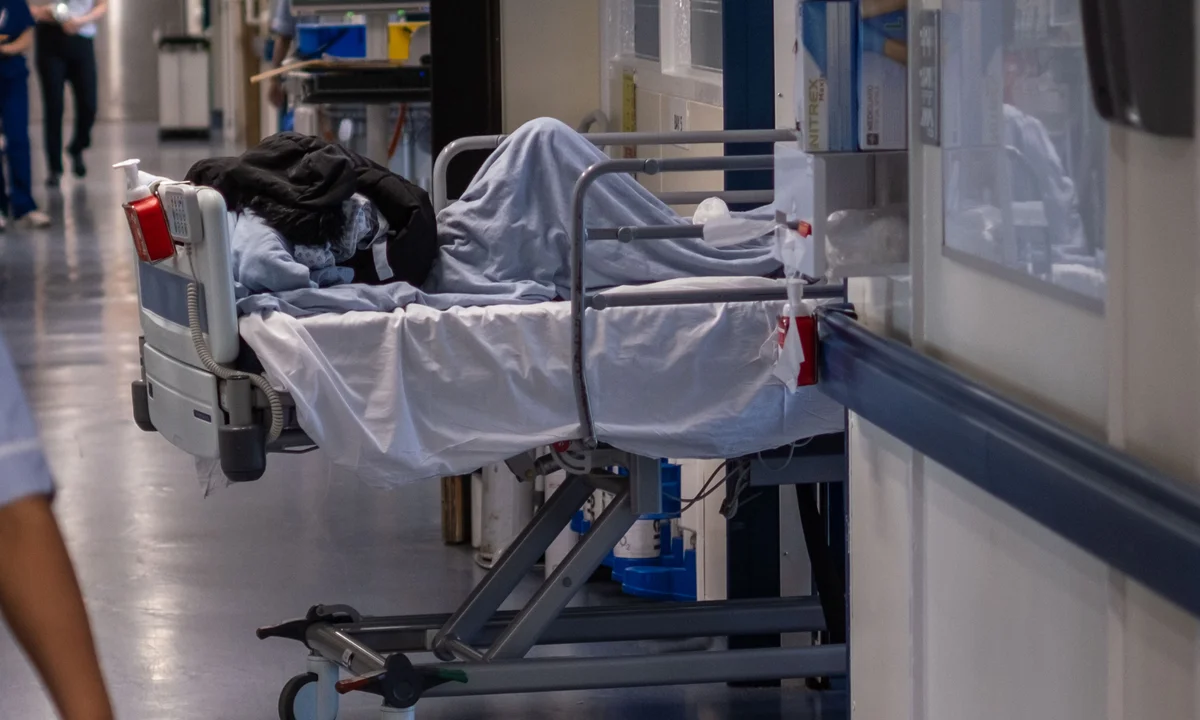
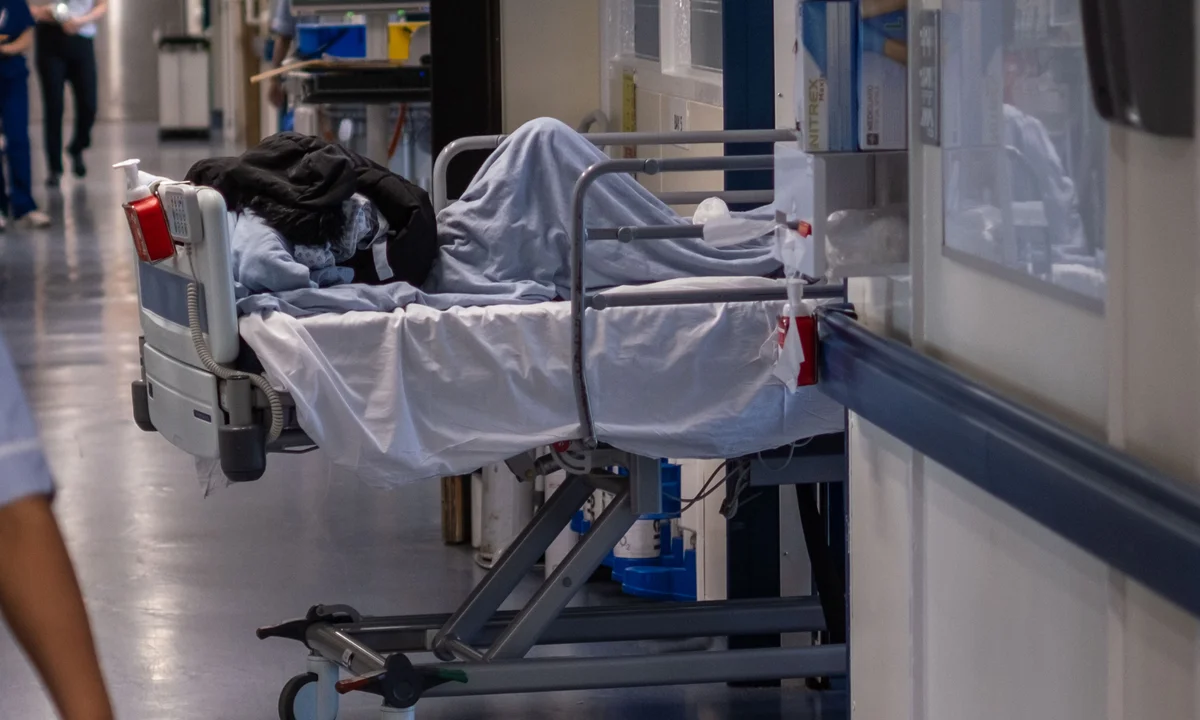
For patients, corridor care is often undignified and unsafe. Testimonies collected in early January 2026 describe harrowing scenes of patients sitting in chairs for days, beds lining busy passageways, and staff improvising privacy for sensitive procedures. Reports, including recent ITV News coverage, have detailed elderly patients spending multiple days in A&E corridors and makeshift areas while waiting for a proper hospital bed. Patients and families have described the experience as "mental cruelty" and traumatic. The Royal College of Nursing (RCN) has called corridor care a "type of torture," warning that it contributes to avoidable deaths and profound psychological distress for both patients and clinicians, citing the tragic case of an elderly patient who choked to death in a corridor. Public concern mirrors the professional alarm, with a poll finding that almost one in five people in England had recently received or witnessed corridor care.
The crisis is driven by multiple systemic factors. High winter demand from flu, norovirus, and other seasonal infections is coupled with persistently limited community and social care capacity. This combination leaves patients stranded in hospital, despite being ready for discharge, contributing to the emergency care backlog and long waits for hospital admission which remain at record highs. Professional bodies have been vocal in their demands. The Royal College of Emergency Medicine (RCEM) and RCN have strongly voiced alarm at the conditions, with Dr Ian Higginson of RCEM describing corridor care as "the most visible symptom of a health service struggling." Even the Health Services Safety Investigations Body (HSSIB) has noted that hospitals are now installing basic infrastructure in corridors and offices because they cannot avoid using these spaces. Although NHS England guidance firmly states that corridor care is unacceptable and must never become ‘business as usual,’ the practice persists.
Political and professional leaders have set an ambitious, though challenging, target to end corridor care by 2029. Tackling the issue requires a dual approach of short-term mitigation and long-term reform, focusing on expanding bed capacity, strengthening community care to prevent admissions, and enhancing patient flow throughout the system. In the bleak context of winter 2026, corridor care remains a vivid illustration of systemic strain across the NHS—a distressing sign that, despite isolated performance gains, the urgent and emergency pathways are failing to consistently deliver safe and dignified care.